ABOUT BONE MARROW TRANSPLANT
A bone marrow transplant is performed to replace damaged or destroyed bone marrow. Bone marrow may stop functioning as a result of diseases such as aplastic anemia or sickle cell anemia, or from being destroyed by chemotherapy or radiation therapy used to treat cancer or other diseases.
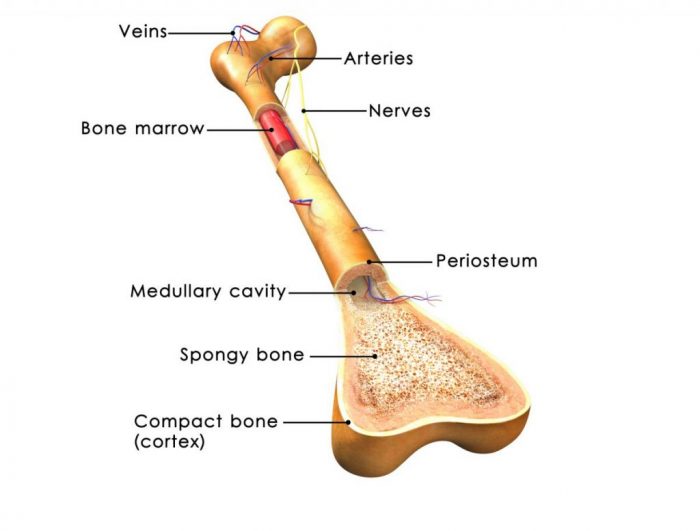
Bone marrow is the spongey tissue located inside the bones in the body. It is made up of stem cells. These stem cells produce other blood cells, such as white cells to fight against infection and red cells and platelets, which help the blood to clot and to circulate oxygen throughout the body.
There are 3 different types of bone marrow transplants which are autologous, allogenic, and syngeneic. Autologous bone marrow transplant harvests the patients own bone marrow before receiving chemotherapy or radiation therapy, and stores it in a freezer until the treatment is complete. The healthy bone marrow is then transplanted back to the patient after they are finished with treatment and are in remission.
Allogenic transplants involve taking the bone marrow from a donor, which is commonly a family member, and transplanting this to the patient. Syngeneic transplants involve taking bone marrow from the patient’s identical twin or from an umbilical cord and transplanting it to the patient.
Recommended for
- Leukemia
- Aplastic anemia
- Lymphoma
- Patients who have had chemotherapy which has destroyed the bone marrow
- Sickle cell anemia
- Autoimmune diseases such as MS
TIME REQUIREMENTS
- Average length of stay abroad: 4 – 8 weeks.
The length of hospital stay required varies with each type of transplant performed and with each patient.
- Number of trips abroad needed: 1.

HOW TO FIND QUALITY TREATMENT ABROAD
BEFORE BONE MARROW TRANSPLANT ABROAD
Before receiving a bone marrow transplant, patients will undergo an extensive evaluation to ensure that it is the best option for them.
A series of tests will be performed to ensure the patient is healthy enough to receive the transplant and they will usually need to arrive at the clinic or hospital around 10 days before the transplant, to have a central line fitted in their chest, in preparation for the transplant.
For the donor, they must also undergo a series of tests and evaluations to ensure that they are the correct match for the recipient. The donor is usually given medication prior to donating the bone marrow as a means of increasing bone marrow production.
The bone marrow is then harvested from the donor, usually from the hip or sternum using a needle. Alternatively, the bone marrow can be collected from peripheral blood stem cells, which involves extracting blood and filtering it through a machine that withdraws the stem cells, and returns the remaining blood back to the donor. Often times, the the bone marrow is taken from the patient before treatment and then returned back to them, rather than using a donor.
Patients with complex conditions may benefit from seeking a second opinion before beginning a treatment plan. A second opinion means that another doctor, usually an expert with a lot of experience, will review the patient’s medical history, symptoms, scans, test results, and other important information, in order to provide a diagnosis and treatment plan. When asked, 45% of US residents who received a second opinion said that they had a different diagnosis, prognosis, or treatment plan.
HOW IS IT PERFORMED
Chemotherapy or radiation therapy is often used as part of the process to treat the cancer or disease in the bone marrow and to make room for bone marrow transplant by destroying the damaged bone marrow.
Once this phase is complete, the bone marrow is then transplanted to the patient into the blood, through the central line in their chest. The new stem cells will travel via the blood to the bone marrow and begin to produce new and healthy cells.
Anesthesia
General anesthetic
WHAT TO EXPECT AFTER BONE MARROW TRANSPLANT
Post procedure care
Patients will need to spend a few weeks in the hospital after the procedure, in order to recover. Regular blood counts will be taken in the proceeding days after the transplant and blood transfusions may be needed.
In the case where an allogeneic transplant has been performed, the patient is usually given medication to take as a precaution to preventing graft-versus-host-disease, whereby the new cells may begin to attack the patient’s tissue.
Recovery from the transplant can take months after the patient leaves the hospital and they will need to attend regular check-ups.
IMPORTANT THINGS TO KNOW ABOUT BONE MARROW TRANSPLANT
Potential risks
- Chest pain
- Fever
- Nausea
- Headache
- Low blood pressure
- Anemia
- Infection
- Graft failure
- Graft-versus-host-disease
FREQUENTLY ASKED QUESTIONS
The transplant procedure is performed under anesthesia, therefore you will not feel any pain. Before the procedure, the recipient patient (the one receiving the transplant) undergoes a process called “conditioning” where the body’s immune system is suppressed and, if they are being treated for malignant cancer, cancer cells are destroyed, using chemotherapy and radiation. The conditioning process can cause some painful side-effects that will be mitigated as much as possible with medication.
Bone marrow transplant uses stem cells to replace damaged or diseased bone marrow in patients with a variety of diseases. It also helps patients undergoing aggressive chemotherapy or radiation therapy continue treatment safely.
More than 50,000 bone marrow transplants are performed world-wide every year according to the World Health Organization.
They are different names for essentially the same treatment. Bone marrow transplants are taking advantage of the stem cells in bone marrow. Sometimes, the stem cells can come from sources other than bone marrow so they’re simply called stem cell transplants or stem cell therapy.
A bone marrow transplant presents significant risks. There are many factors influencing the risk of complications, and you should discuss them further with your specialist. Some of the potential complications include graft-versus-host disease (allogenic transplants only), graft (transplant) failure, organ damage, infections, cataracts, infertility, and increased risk of cancer.
Bone marrow transplant is one part of treating leukemia, and the results vary dramatically for individual patients.










